How to Calculate When Baby Will Be Born by the Measurement of the Embryo
Gestational age is a measure of the age of a pregnancy which is taken from the beginning of the woman's final menstrual period (LMP), or the respective historic period of the gestation as estimated by a more than accurate method if available. Such methods include adding xiv days to a known duration since fertilization (every bit is possible in in vitro fertilization), or by obstetric ultrasonography. The popularity of using such a definition of gestational age is that menstrual periods are essentially always noticed, while in that location is unremarkably a lack of a convenient way to discern when fertilization occurred.
The initiation of pregnancy for the adding of gestational age can be unlike from definitions of initiation of pregnancy in context of the abortion debate or get-go of human personhood.
Methods [edit]
Co-ordinate to American College of Obstetricians and Gynecologists, the main methods to calculate gestational age are:[1]
- Directly calculating the days since the beginning of the last menstrual period
- Early obstetric ultrasound, comparing the size of an embryo or fetus to that of a reference group of pregnancies of known gestational age (such as calculated from last menstrual periods) and using the mean gestational age of other embryos or fetuses of the same size. If the gestational age as calculated from an early ultrasound is contradictory to the one calculated direct from the last menstrual menstruation, it is still the one from the early on ultrasound that is used for the residue of the pregnancy.[1]
- In instance of in vitro fertilization, calculating days since oocyte retrieval or co-incubation and adding 14 days.[2]
Gestational age tin also be estimated past calculating days from ovulation if information technology was estimated from related signs or ovulation tests, and adding xiv days by convention.[3]
A more consummate list of methods is given in post-obit tabular array:[4]
| Method of estimating gestational historic period | Variability (two standard deviations)[four] |
|---|---|
| Days from oocyte retrieval or co-incubation in in vitro fecundation + 14 days | ±one solar day |
| Days from estimated ovulation in Ovulation induction + 14 days | ±3 days |
| Days from artificial insemination + xiv days | ±three days |
| Days from known single sexual intercourse + 14 days | ±3 days |
| Days from estimated ovulation by basal body temperature record + xiv days | ±4 days |
| Outset-trimester physical examination | ±2 weeks |
| Second-trimester physical examination | ±iv weeks |
| 3rd-trimester physical examination | ±vi weeks |
| First-trimester obstetric ultrasonography (crown-rump length) | ±8% of the judge |
| Second-trimester obstetric ultrasonography (caput circumference, femur length) | ±8% of the guess |
| Third-trimester obstetric ultrasonography (caput circumference, femur length) | ±8% of the estimate |
As a general dominion, the official gestational age should be based on the actual beginning of the last menstrual period, unless any of the above methods gives an estimated date that differs more than than the variability for the method, in which case the difference cannot probably be explained by that variability alone.[four] For example, if there is a gestational age based on the beginning of the last menstrual period of nine.0 weeks, and a commencement-trimester obstetric ultrasonography gives an estimated gestational age of x.0 weeks (with a two SD variability of ±eight% of the estimate, thereby giving a variability of ±0.8 weeks), the difference of 1.0 weeks between the tests is larger than the 2 SD variability of the ultrasonography estimate, indicating that the gestational historic period estimated by ultrasonography should be used every bit the official gestational historic period.[4]
Once the estimated due engagement (EDD) is established, information technology should rarely be changed, as the determination of gestational age is most authentic earlier in the pregnancy.[5]
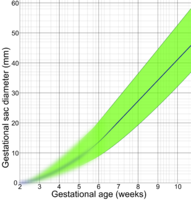
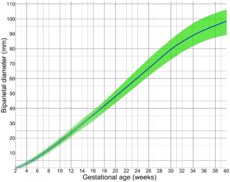
Following are diagrams for estimating gestational age from obstetric ultrasound, by various target parameters:
Comparison to fertilization age [edit]
The fertilization or conceptional age (also called embryonic age and later fetal age) is the time from the fertilization. It usually occurs within a twenty-four hours of ovulation, which, in turn, occurs on boilerplate 14.6 days afterward the beginning of the preceding menstruation (LMP). There is also considerable variability in this interval, with a 95% prediction interval of the ovulation of 9 to xx days afterward catamenia even for an average woman who has a mean LMP-to-ovulation time of fourteen.6.[7] In a reference group representing all women, the 95% prediction interval of the LMP-to-ovulation is viii.2 to xx.5 days. The actual variability between gestational age as estimated from the beginning of the terminal menstrual period (without the use of any boosted method mentioned in previous section) is substantially larger because of uncertainty which menstrual cycle gave rise to the pregnancy. For example, the period may be deficient enough to give the false appearance that an earlier flow gave ascent to the pregnancy, potentially giving an estimated gestational age that is approximately one calendar month too large. Also, vaginal bleeding occurs during 15-25% of first trimester pregnancies,[8] and may be mistaken as menstruum, potentially giving an estimated gestational age that is also low.
Uses [edit]
Gestational age is used for example for:[ citation needed ]
- The events of prenatal development, which ordinarily occur at specific gestational ages. Hence, the gestational timing of a fetal toxin exposure, fetal drug exposure or vertically transmitted infection can be used to predict the potential consequences to the fetus.
- Estimated date of delivery
- Scheduling prenatal care
- Interpretation of fetal viability
- Computing the results of various prenatal tests, (for example, in the triple examination).
- Nativity classification into for example preterm, term or postterm.
- Classification of infant deaths and stillbirths
- Postnatally (later birth) to estimate various risk factors

Timeline of pregnancy by gestational age.
Estimation of due engagement [edit]

Distribution of gestational age at childbirth amidst singleton live births, given both when gestational age is estimated by showtime trimester ultrasound and straight by last menstrual menstruum[9]
The mean pregnancy length has been estimated to be 283.4 days of gestational historic period every bit timed from the beginning day of the final menstrual period and 280.six days when retrospectively estimated by obstetric ultrasound measurement of the fetal biparietal bore (BPD) in the second trimester.[10] Other algorithms accept into account other variables, such as whether this is the offset or subsequent child, the female parent's race, age, length of menstrual cycle, and menstrual regularity. In order to take a standard reference point, the normal pregnancy duration is assumed by medical professionals to be 280 days (or 40 weeks) of gestational age. Furthermore, actual childbirth has only a sure probability of occurring within the limits of the estimated due date. A written report of singleton live births came to the effect that childbirth has a standard departure of 14 days when gestational age is estimated by first-trimester ultrasound and 16 days when estimated straight past terminal menstrual menstruum.[ix]
The most common system used among healthcare professionals is Naegele'south rule, which estimates the expected engagement of commitment (EDD) past adding a year, subtracting three months, and calculation 7 days to the beginning day of a woman's last menstrual period (LMP) or corresponding date as estimated from other ways.
Medical fetal viability [edit]
In that location is no precipitous limit of development, gestational historic period, or weight at which a human fetus automatically becomes viable.[xi] According to studies between 2003 and 2005, xx to 35 percent of babies born at 23 weeks of gestation survive, while 50 to 70 percent of babies born at 24 to 25 weeks, and more than ninety percent born at 26 to 27 weeks, survive.[12] It is rare for a baby weighing less than 500 g (17.6 ounces) to survive.[11] A baby'due south chances for survival increases three-4% per twenty-four hours between 23 and 24 weeks of gestation and about 2-3% per day between 24 and 26 weeks of gestation. Afterwards 26 weeks the charge per unit of survival increases at a much slower rate because survival is high already.[13] Prognosis depends also on medical protocols on whether to resuscitate and aggressively treat a very premature newborn, or whether to provide only palliative care, in view of the high risk of severe disability of very preterm babies.[fourteen]
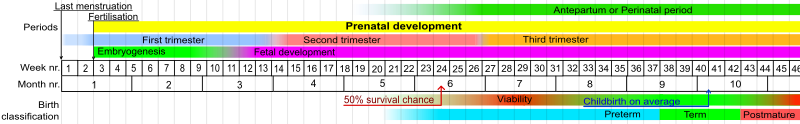
Stages in prenatal development, showing viability and point of 50% chance of survival (limit of viability) at bottom. Weeks and months numbered past gestation,
| Completed weeks of gestation at birth | 21 and less | 22 | 23 | 24 | 25 | 26 | 27 | 30 | 34 |
|---|---|---|---|---|---|---|---|---|---|
| Chance of survival[13] | 0% | 0–10% | 10–35% | 40–seventy% | 50–80% | lxxx–90% | >90% | >95% | >98% |
Birth nomenclature [edit]
Using gestational age, births can be classified into wide categories:
| Gestational Age in Weeks | Classification |
|---|---|
| < 37 0/7 | Preterm |
| 34 0/7 - 36 half dozen/vii | Tardily preterm[15] |
| 37 0/vii - 38 6/7 | Early Term[16] |
| 39 0/7 - 40 6/7 | Full Term[16] |
| 41 0/7 - 41 6/7 | Late Term[sixteen] |
| > 42 0/7 | Postterm |
Using the LMP (last menstrual period) method, a full-term human pregnancy is considered to be 40 weeks (280 days), though pregnancy lengths between 38 and 42 weeks are considered normal. A fetus born prior to the 37th calendar week of gestation is considered to exist preterm. A preterm infant is likely to be premature and consequently faces increased risk of morbidity and mortality. An estimated due engagement is given by Naegele's dominion.
Co-ordinate to the WHO, a preterm nativity is defined as "babies built-in live before 37 weeks of pregnancy are completed."[17] According to this classification, at that place are three sub-categories of preterm birth, based on gestational age: extremely preterm (fewer than 28 weeks), very preterm (28 to 32 weeks), moderate to late preterm (32 to 37 weeks).[17] Various jurisdictions may use unlike classifications.
In classifying perinatal deaths, stillbirths and infant deaths [edit]
For most of the 20th Century, official definitions of a live birth and infant death in the Soviet Union and Russia differed from common international standards, such as those established by the Earth Health Organization in the latter role of the century.[eighteen] [19] Babies who were fewer than 28 weeks of gestational age, or weighed fewer than 1000 grams, or fewer than 35 cm in length – even if they showed some sign of life (breathing, heartbeat, voluntary muscle movement) – were classified as "alive fetuses" rather than "alive births." Only if such newborns survived seven days (168 hours) were they and then classified equally live births. If, however, they died within that interval, they were classified as stillbirths. If they survived that interval merely died within the first 365 days they were classified as infant deaths.
More recently, thresholds for "fetal death" proceed to vary widely internationally, sometimes incorporating weight as well as gestational age. The gestational age for statistical recording of fetal deaths ranges from xvi weeks in Kingdom of norway, to 20 weeks in the US and Australia, 24 weeks in the UK, and 26 weeks in Italy and Spain.[20] [21] [22]
The WHO defines the perinatal period as "The perinatal period commences at 22 completed weeks (154 days) of gestation and ends seven completed days later nascence."[23] Perinatal mortality is the decease of fetuses or neonates during the perinatal period. A 2013 study institute that "While merely a modest proportion of births occur before 24 completed weeks of gestation (about 1 per m), survival is rare and well-nigh of them are either fetal deaths or live births followed by a neonatal death."[20]
Postnatal utilize [edit]
Gestational historic period (as well as fertilization historic period) is sometimes used postnatally (after birth) to estimate various take a chance factors. For example, it is a improve predictor than postnatal historic period for risk of intraventricular hemorrhage in premature babies treated with extracorporeal membrane oxygenation.[24]
Factors affecting pregnancy length [edit]
Child's gestational age at birth (pregnancy length) is associated with various probable causal maternal non-genetic factors: stress during pregnancy,[25] age, parity, smoking, infection and inflammation, BMI. Also, preexisting maternal medical conditions with genetic component, east.g., diabetes mellitus type 1, systemic lupus erythematosus, anaemia. Parental ancestral groundwork (race) also plays a office in pregnancy duration. Gestational age at nascency is on average shortened by various pregnancy aspects: twin pregnancy, prelabor rupture of (fetal) membranes, pre-eclampsia, eclampsia, intrauterine growth restriction.[26] The ratio between fetal growth rate and uterine size (reflecting uterine distension) is suspected to partially make up one's mind the pregnancy length.[27]
Heritability of pregnancy length [edit]
Family-based studies showed that gestational historic period at nascency is partially (from 25% to twoscore%) determined by genetic factors.[28]
Run across too [edit]
- Pregnancy
- Motherhood
- Prenatal evolution
- Gestation periods in mammals
- Ballgame law
- Reproductive rights
- Fetal rights
References [edit]
- ^ a b Obstetric Data Definitions Issues and Rationale for Alter - Gestational Age & Term Archived 2013-xi-06 at the Wayback Car from Patient Safety and Quality Improvement at American Congress of Obstetricians and Gynecologists. Created November 2012.
- ^ Tunon, K.; Eik-Nes, S. H.; Grøttum, P.; Von Düring, V.; Kahn, J. A. (2000). "Gestational age in pregnancies conceived after in vitro fertilization: A comparison between historic period assessed from oocyte retrieval, crown-rump length and biparietal diameter". Ultrasound in Obstetrics and Gynecology. 15 (1): 41–46. doi:10.1046/j.1469-0705.2000.00004.x. PMID 10776011. S2CID 20029116.
- ^ Robinson, H. P.; Fleming, J. E. Eastward. (1975). "A Disquisitional Evaluation of Sonar "crown-Rump Length" Measurements". BJOG: An International Journal of Obstetrics and Gynaecology. 82 (9): 702–10. doi:x.1111/j.1471-0528.1975.tb00710.ten. PMID 1182090. S2CID 31663686.
- ^ a b c d A Uncomplicated Solution to Dating Discrepancies: The Rule of Eights Hunter, Fifty. A. (2009). "Issues in Pregnancy Dating: Revisiting the Evidence". Journal of Midwifery & Women'southward Health. 54 (3): 184–190. doi:10.1016/j.jmwh.2008.11.003. PMID 19410210.
- ^ "Committee Opinion No 611". Obstetrics & Gynecology. 124 (4): 863–866. 2014. doi:x.1097/01.AOG.0000454932.15177.be. PMID 25244460.
- ^ Derived from a standard deviation in this interval of ii.6, equally given in: Fehring RJ, Schneider Yard, Raviele One thousand (2006). "Variability in the phases of the menstrual bike". J Obstet Gynecol Neonatal Nurs. 35 (3): 376–84. doi:10.1111/j.1552-6909.2006.00051.x. PMID 16700687.
- ^ Snell, BJ (Nov–Dec 2009). "Cess and direction of bleeding in the beginning trimester of pregnancy". Journal of Midwifery & Women's Health. 54 (vi): 483–91. doi:ten.1016/j.jmwh.2009.08.007. PMID 19879521.
- ^ a b Hoffman, Caroline South.; Messer, Lynne C.; Mendola, Pauline; Savitz, David A.; Herring, Amy H.; Hartmann, Katherine Eastward. (2008). "Comparing of gestational historic period at birth based on last menstrual menses and ultrasound during the showtime trimester". Paediatric and Perinatal Epidemiology. 22 (half-dozen): 587–596. doi:ten.1111/j.1365-3016.2008.00965.10. ISSN 0269-5022. PMID 19000297.
- ^ Kieler, H; Axelsson, O; Nilsson, S; Waldenströ, U (1995). "The length of man pregnancy as calculated by ultrasonographic measurement of the fetal biparietal diameter". Ultrasound in Obstetrics and Gynecology. 6 (5): 353–7. doi:10.1046/j.1469-0705.1995.06050353.x. PMID 8590208. S2CID 39447672.
- ^ a b Moore, Keith and Persaud, T. The Developing Homo: Clinically Oriented Embryology, p. 103 (Saunders 2003).
- ^ March of Dimes --> Neonatal Death Retrieved on Nov 10, 2014. In turn citing:
- Tyson JE, Parikh NA, Langer J, Green C, Higgins RD (April 2008). "Intensive care for farthermost prematurity--moving beyond gestational age". N. Engl. J. Med. 358 (xvi): 1672–81. doi:10.1056/NEJMoa073059. PMC2597069. PMID 18420500.
- Luke B, Brown MB (December 2006). "The changing risk of baby bloodshed past gestation, plurality, and race: 1989-1991 versus 1999-2001". Pediatrics. 118 (6): 2488–97. doi:10.1542/peds.2006-1824. PMC3623686. PMID 17142535.
- The American Higher of Obstetricians and Gynecologists (September 2002). "ACOG Practice Bulletin: Clinical Direction Guidelines for Obstetrcian-Gynecologists: Number 38, September 2002. Perinatal intendance at the threshold of viability". Obstet Gynecol. 100 (3): 617–24. doi:x.1016/S0029-7844(02)02260-3. PMID 12220792.
- ^ a b (). What are the chances that my infant will survive?. [ONLINE] Available at: http://www.spensershope.org/chances_for_survival.htm Archived 2018-08-09 at the Wayback Machine. [Final Accessed fourteen Nov 2012].
- ^ Verlato, Giovanna; Gobber, Daniela; Drago, Donatella; Chiandetti, Lino; Drigo, Paola; Working Grouping of Intensive Intendance in the Delivery Room of Extremely Premature Newborns (2016). "Guidelines for Resuscitation in the Delivery Room of Extremely Preterm Infants". Journal of Child Neurology. 19 (1): 31–iv. doi:10.1177/088307380401900106011. PMID 15032380. S2CID 20200767.
- ^ Late-Preterm Infants Archived 2012-05-02 at the Wayback Auto ACOG Committee Opinion 404
- ^ a b c Ob-Gyns Redefine Significant of "Term Pregnancy" Archived 2017-05-03 at the Wayback Car, from American Higher of Obstetricians and Gynecologists. October 22, 2013
- ^ a b [ane][ total citation needed ]
- ^ Anderson, Barbara A; Argent, Brian D (1986). "Babe Mortality in the Soviet Spousal relationship: Regional Differences and Measurement Issues". Population and Development Review. 12 (4): 705–38. doi:10.2307/1973432. JSTOR 1973432.
- ^ Anderson, Barbara A.; Silver, Brian D. (1994). "The Geodemography of Infant Bloodshed in the Soviet Spousal relationship, 1950-1990". PSC Research Report No. 94-316: eight.
- ^ a b Mohangoo, Ashna D; Blondel, Béatrice; Gissler, Mika; Velebil, Petr; MacFarlane, Alison; Zeitlin, Jennifer (2013). "International Comparisons of Fetal and Neonatal Mortality Rates in Loftier-Income Countries: Should Exclusion Thresholds Be Based on Birth Weight or Gestational Historic period?". PLOS 1. eight (v): e64869. Bibcode:2013PLoSO...864869M. doi:10.1371/journal.pone.0064869. PMC3658983. PMID 23700489.
- ^ Li, Z; Zeki, R; Hilder, L; Sullivan, EA (2012). "Australia'due south Mothers and Babies 2010". Perinatal statistics series no. 27. Cat. no. PER 57. Australian Found of Wellness and Welfare National Perinatal Statistics Unit, Australian Government. Retrieved four July 2013.
- ^ Royal College of Obstetricians; Gynaecologists Britain (April 2001). "Further Issues Relating to Tardily Abortion, Fetal Viability and Registration of Births and Deaths". Royal College of Obstetricians and Gynaecologists United kingdom. Archived from the original on 5 November 2013. Retrieved 4 July 2013.
- ^ [2][ full citation needed ]
- ^ Jobe, Alan H (2004). "Mail-conceptional age and IVH in ECMO patients". The Journal of Pediatrics. 145 (2): A2. doi:ten.1016/j.jpeds.2004.07.010.
- ^ Dole, N.; Savitz, D. A.; Hertz-Picciotto, I.; Siega-Riz, A. 1000.; McMahon, G. J.; Buekens, P. (2003-01-01). "Maternal stress and preterm birth". American Periodical of Epidemiology. 157 (1): xiv–24. doi:10.1093/aje/kwf176. ISSN 0002-9262. PMID 12505886.
- ^ Goldenberg, Robert L.; Culhane, Jennifer F.; Iams, Jay D.; Romero, Roberto (2008-01-05). "Epidemiology and causes of preterm nativity". Lancet. 371 (9606): 75–84. doi:10.1016/S0140-6736(08)60074-4. ISSN 1474-547X. PMC7134569. PMID 18177778.
- ^ Bacelis, Jonas; Juodakis, Julius; Waldorf, Kristina M. Adams; Sengpiel, Verena; Muglia, Louis J.; Zhang, Ge; Jacobsson, Bo (2018-10-01). "Uterine distention every bit a factor in nativity timing: retrospective nationwide cohort study in Sweden". BMJ Open. 8 (ten): e022929. doi:ten.1136/bmjopen-2018-022929. ISSN 2044-6055. PMC6252709. PMID 30385442.
- ^ Clausson, Britt; Lichtenstein, Paul; Cnattingius, Sven (2000). "Genetic influence on birthweight and gestational length adamant by studies in offspring of twins". BJOG. 107 (3): 375–81. doi:10.1111/j.1471-0528.2000.tb13234.ten. PMID 10740335. S2CID 43470321.
Source: https://en.wikipedia.org/wiki/Gestational_age

0 Response to "How to Calculate When Baby Will Be Born by the Measurement of the Embryo"
Post a Comment